How Covid-19 exposed universal healthcare issues: A comparison between the US and Germany
Both the USA and Germany count as two of the most industrialized countries on our planet. However, the numbers of Covid-19 cases and deaths differ drastically from each other. Is the German healthcare system really as good as it is portrayed? What changes need to be made to the American healthcare system?
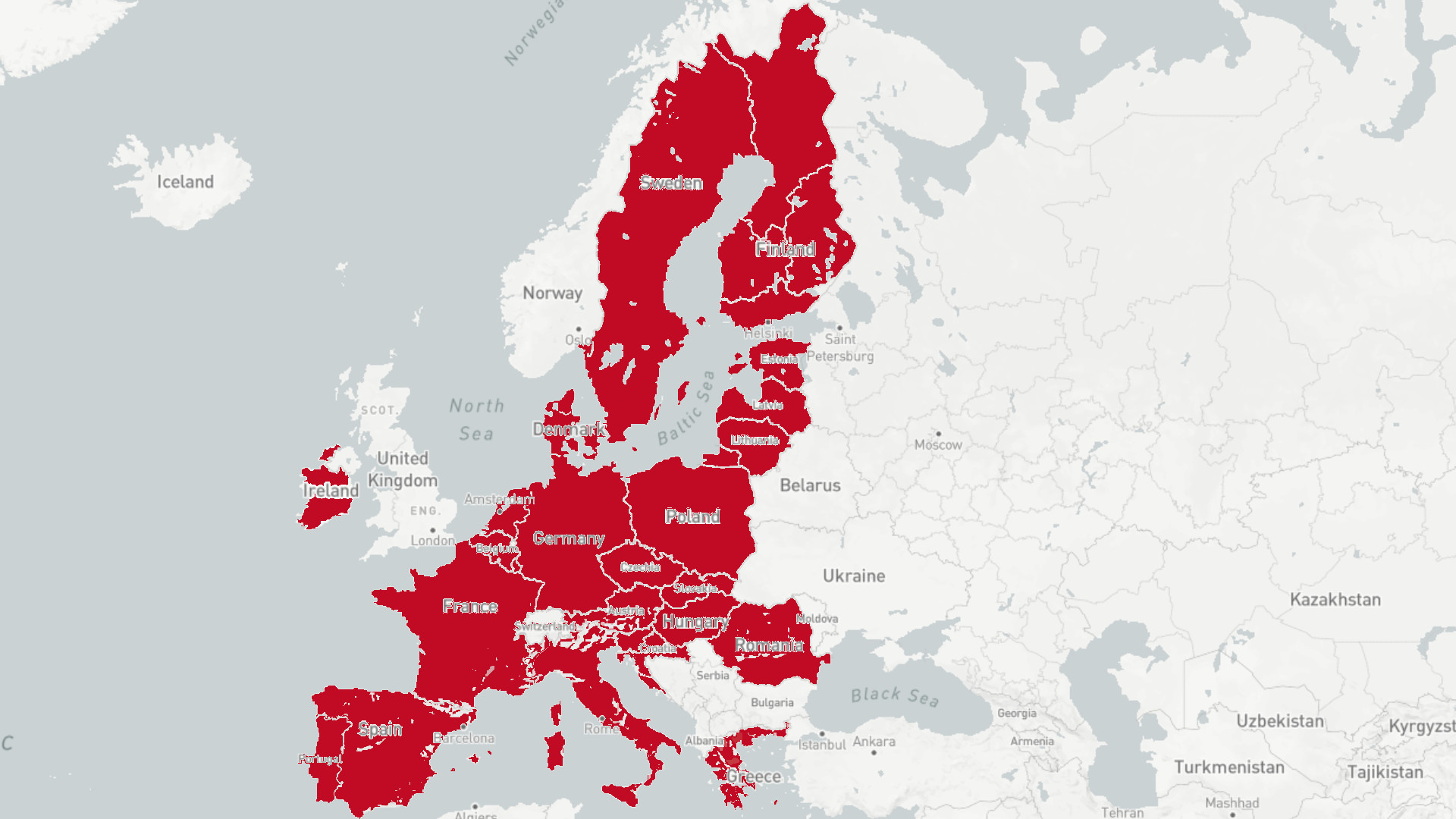
Jens Spahn is a sought-after man, especially these days. In mid-April, the German healthcare minister even appeared on American television. This was a rare occasion for a German politician, but a welcome change for Spahn. Despite the many structural problems German healthcare is facing, Spahn and the German government are praised in foreign countries for their handling of the Covid-19-pandemic. This is mainly due to the fact that Germany has kept the number of deaths low. Despite being hit hard by the virus with almost 196.000 registered cases by the start of July, “only” about 9000 Germans died of the disease, according to the Robert Koch-Institute (RKI). In the United States, the numbers paint a different picture: Almost four times as many Americans died from Covid-19 per 100.000 inhabitants than in Germany – 39 compared to 11, according
to the Johns Hopkins University. Overall, the US registered over 2,7 million cases with more than 129.000 deaths by the start of July. Both the USA and Germany count as two of the most industrialized countries on our planet. However, the numbers of those infected by Covid-19, and the number of deaths related to the virus, differ drastically from each other. How is that possible? Is the German healthcare system really as good as it is portrayed? What changes need to be made to the American healthcare system?
To gain a deeper understanding, it is necessary to take a brief look into the history of the American healthcare system. The system was created at the turn of the late 19th century, and during its earliest phases during the Civil War, the sector was unregulated. It only began to take in federal funding at the end of the 1800s, Gunnar Almgren outlines in his book Health Care Politics, Policy and Services.
In the 1930s, the economic formation of the sector began to evolve towards private insurance plans, while federal investments began to rise. By the turn of the century, following changes to the American landscape post World War II and the Great Depression, the Hill-Burton Act of 1946 was introduced. The act enabled multi-billion dollar federal investments to expand hospitals and healthcare institutions. Through the early 50s, local and state funding hit 9.1 billion, sparked by industrialization, suburbanization and a post-war baby boom. In the mid-60s, Medicare and Medicaid noticed an increase in the number of patients using healthcare services. By the 1970s, a healthcare emergency was declared, as the working poor could not qualify for Medicaid and had difficulties acquiring access to healthcare services. In
1993, President Bill Clinton attempted to develop a universal healthcare system. With this incentive, large insurance companies would benefit from businesses requiring their employees to purchase insurance. By 2010, President Obama signed the Patient Protection and Affordable Care Act into law, a move towards universal coverage. The law outlined penalties for citizens that did not have insurance and expanded Medicaid, Christy Chapin explains in her book Ensuring American’s
Health. But recurring fractures in the system, growing health epidemics, and private and public incentives continue to prevent universal healthcare from becoming a reality.
The history of German health also has a long history. Since 1883, health insurance iscompulsory for every Germany employee. At that time, around ten percent of Germans were covered by statutory insurance. Today, the share has risen to almost 90 percent of the German population, according to the federal ministry of health. In addition, anyone who has a yearly salary of more than 56.250 Euros can opt for private health insurance. The advantage: Earlier appointments, and single rooms in the hospital. Nevertheless, every German has the equal right to medical treatment regardless of whether their insurance is statutory or private. When asked in an interview with NBBC what the secret behind Germany’s success in fighting
Covid-19 was, health minister Spahn referred to the German health care system being in “very good shape”. Furthermore, Spahn mentioned the high number of general practitioners in Germany as a reason for success: “They take care of the less severe cases, to avoid overcrowded hospitals.” In fact, general practitioners are the first contact point for any German citizen needing medical treatment. Overall, Germany has a high density of doctors with 4,3 per 100.000 inhabitants, compared to the US with 2,6, according to the OECD world health report. Moreover, German health insurance covers large parts of medication and hospital stays. Germans pay only a maximum of 10 Euros for their prescription medication, even if the drug originally costs 400 Euros. Any necessary and urgent operation is covered by health insurance as well, and for every additional day in the hospital, Germans pay a fee of only 10 Euros.
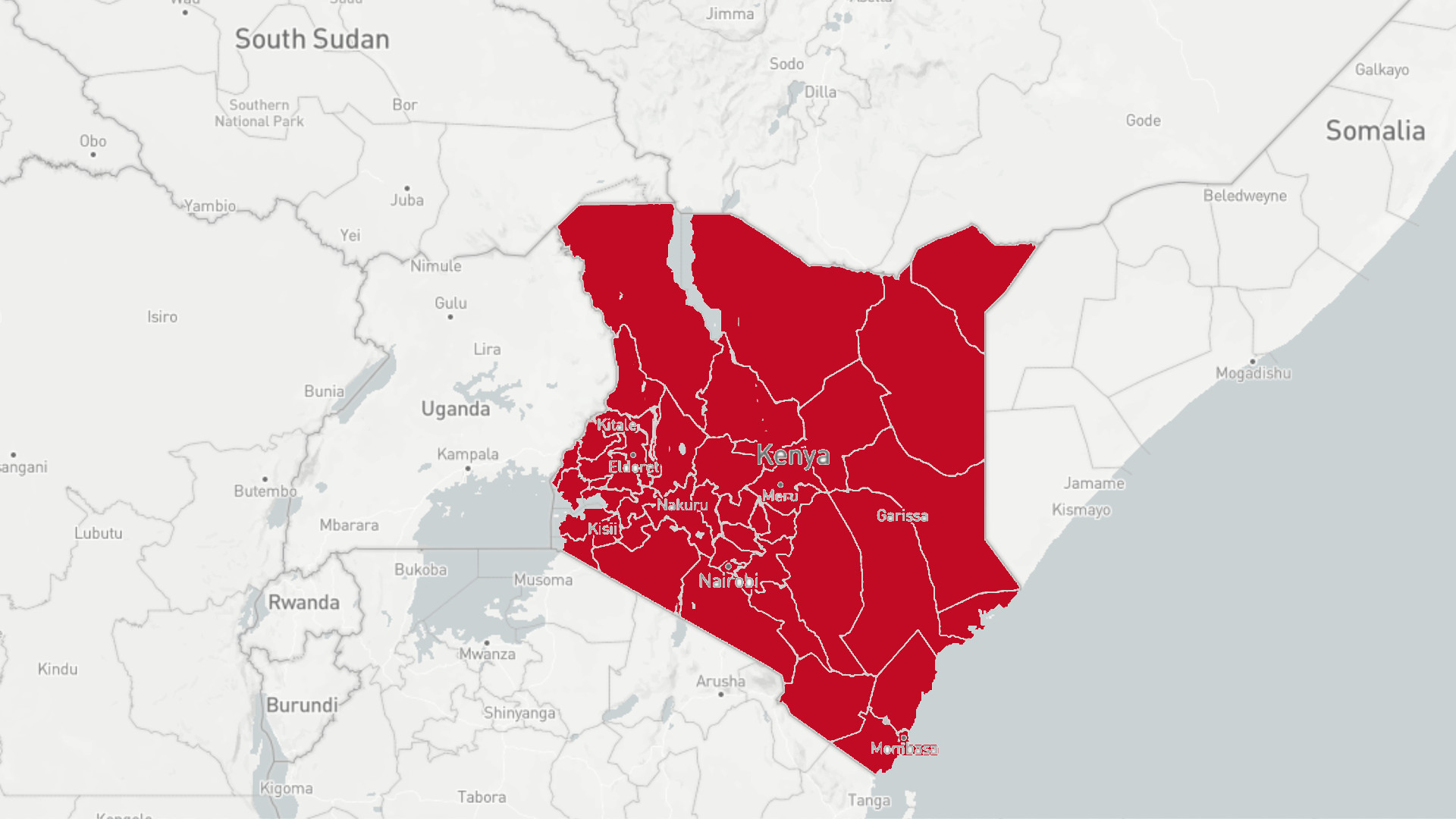
In the United States, Covid-19 has only further exposed the gaps in healthcare. Reports have shown that service-sector workers have been worst affected. Outer lying communities, such as military veterans and indigenous American Indians, also lack the appropriate resources. If workers contract the virus, they face a payout fee of up to $400 for treatment. More than 45% of essential service workers have stated that they will not be able to afford the costs of taking leave if they are infected with the virus. As infections began to rise, there was an economic hit costing $654 billion and $3450 per patient, according to Health Affairs.
In order to offset these costs, there has been a rise in the virtual sphere, where medical doctors and physicians have switched to telehealth. But despite Covid-19 advancing in steps towards biomedicine and other tech-based healthcare incentives, it is clear that the lack of ICU beds, ventilators, and adequate testing has taken its toll with over 2,7 million infections recorded by the start of July.
Despite having an established health care system, German hospitals were also not
fully prepared when the Coronavirus started spreading in late February. The stocks of breathing masks, disinfectants and respirators was quite simply not enough to cope with the fast-increasing numbers of Covid-19-cases. To keep the system running, the federal government had to order millions of breathing masks and thousands of respirators in March and April.
The inadequate state of many German hospitals at the start of the pandemic can be
seen as result of years of lack of funding in the health care system. German hospitals depend on state funding, which is supposed to cover the costs for equipment and medical devices. The problem is: The amount of state funding is far from enough, according to the German hospital association (DKG). In the last ten years, German hospitals would have needed almost 30 billion euros more to tackle all of their urgent investments, the organization stated on its website. In order to keep the clinics running, the necessary money is saved by massively underpaying nursing staff, many of whom have been suffering under severe working conditions for years.
All in all, the German healthcare system is fighting the Coronavirus successfully. Now with over 30.000 intensive care beds, and adequate laboratory and testing capacities, the country can guarantee good medical treatment for all its inhabitants. In the US, not only Covid-19 is challenging the health sector: Heart disease, diabetes, and opioid addictions have rippled through the American population long before and stress the needs for preventive care. American policymakers can take a closer look at Germany’s equilateral system and other
functioning healthcare systems, to ensure a healthier future for the country post-COVID and beyond.